Claims Lack Real-Time Oversight

Claims review happens across fragmented tools

Manual workflows slow down intervention

Transparency data is disconnected from claims

Scaling review requires more headcount

Analytics lag by months, not actionable in the moment

No real-time visibility into claims decisions

Site of care choices happen without employer context

Fiduciary responsibility without fiduciary-grade tools
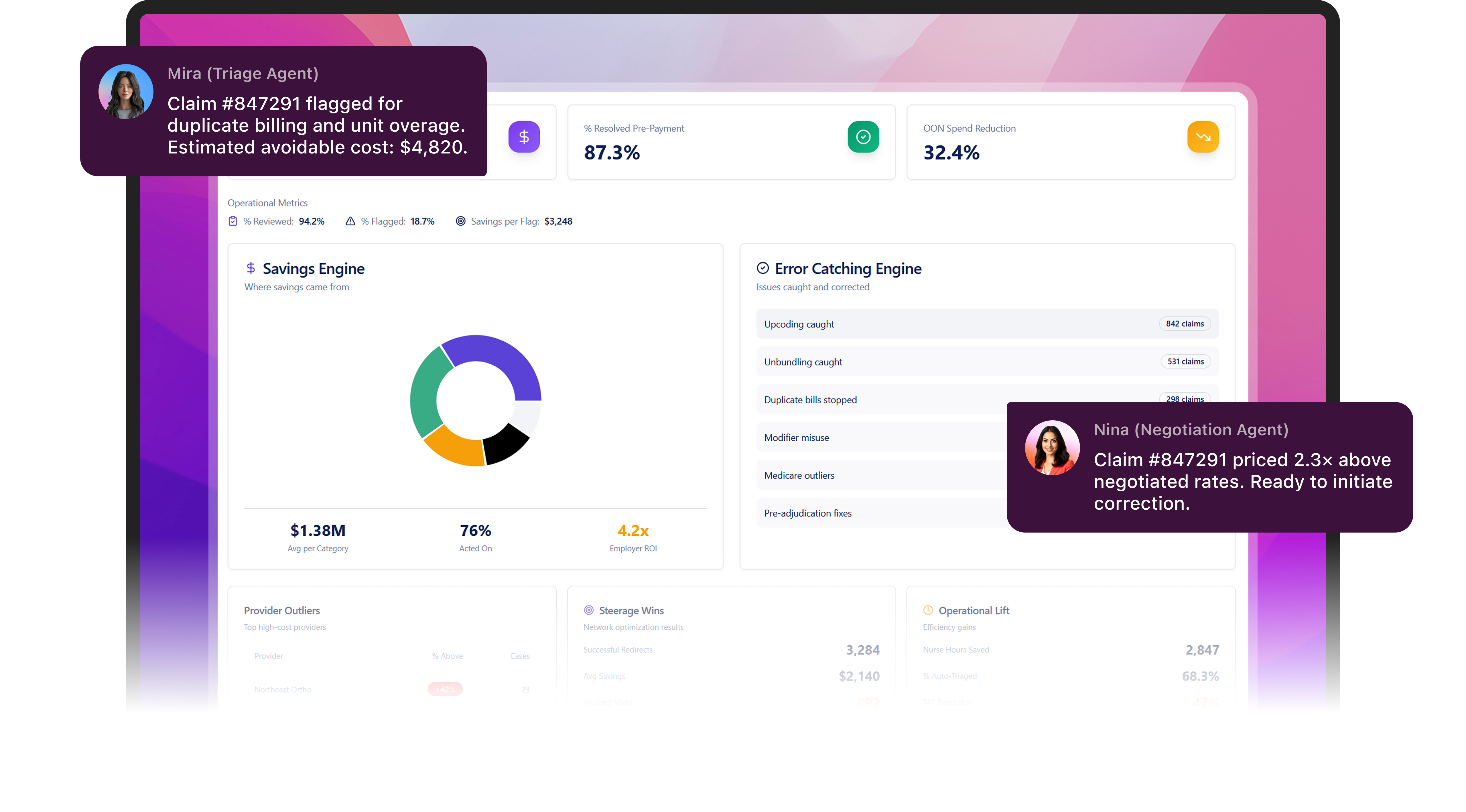
BenOsphere helps TPAs triage and negotiate claims at scale using AI and price transparency data, giving employers fiduciary-grade oversight and measurable savings.
A Claims Triage and Negotiation Platform
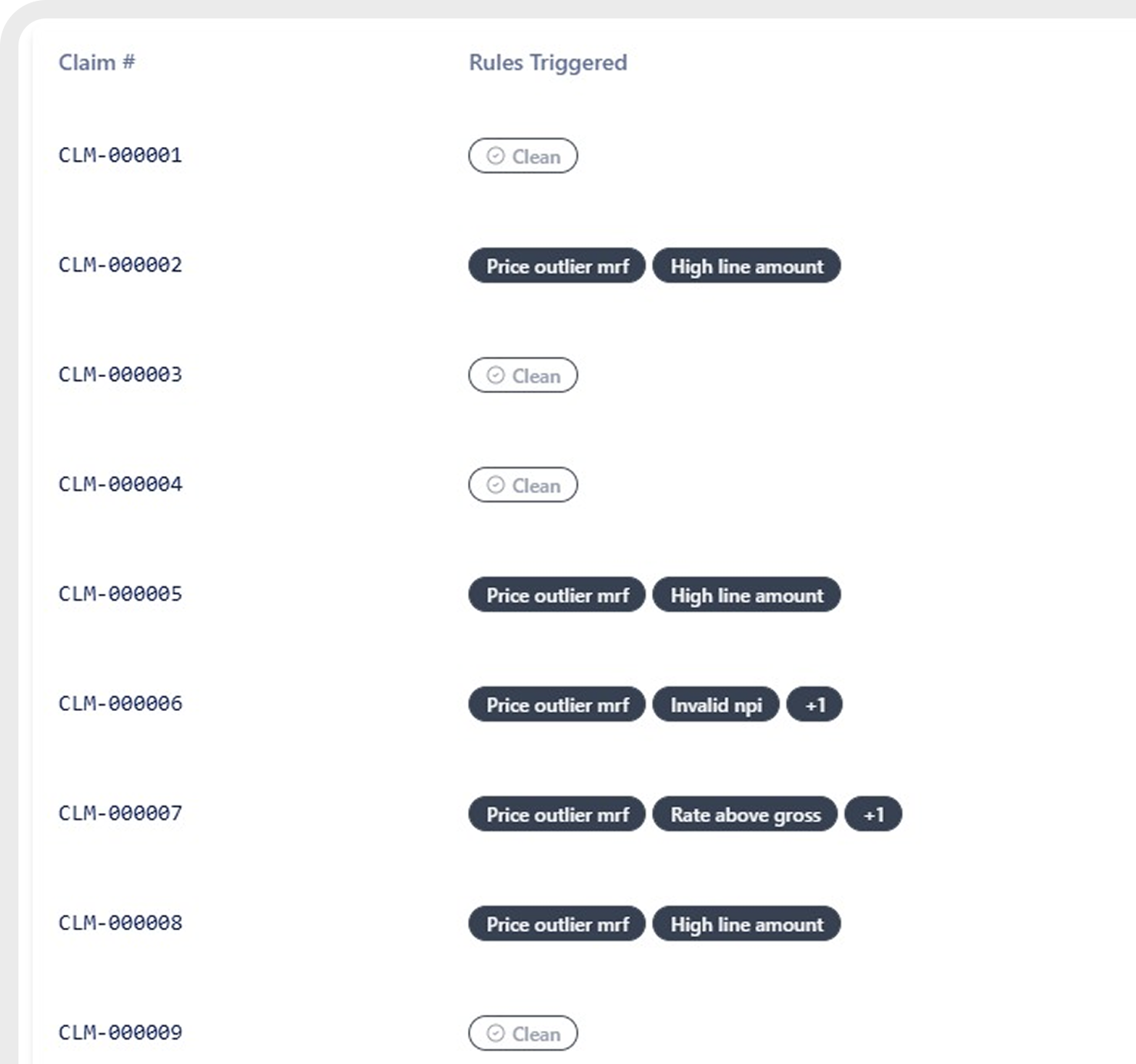
100% Claims. Triaged
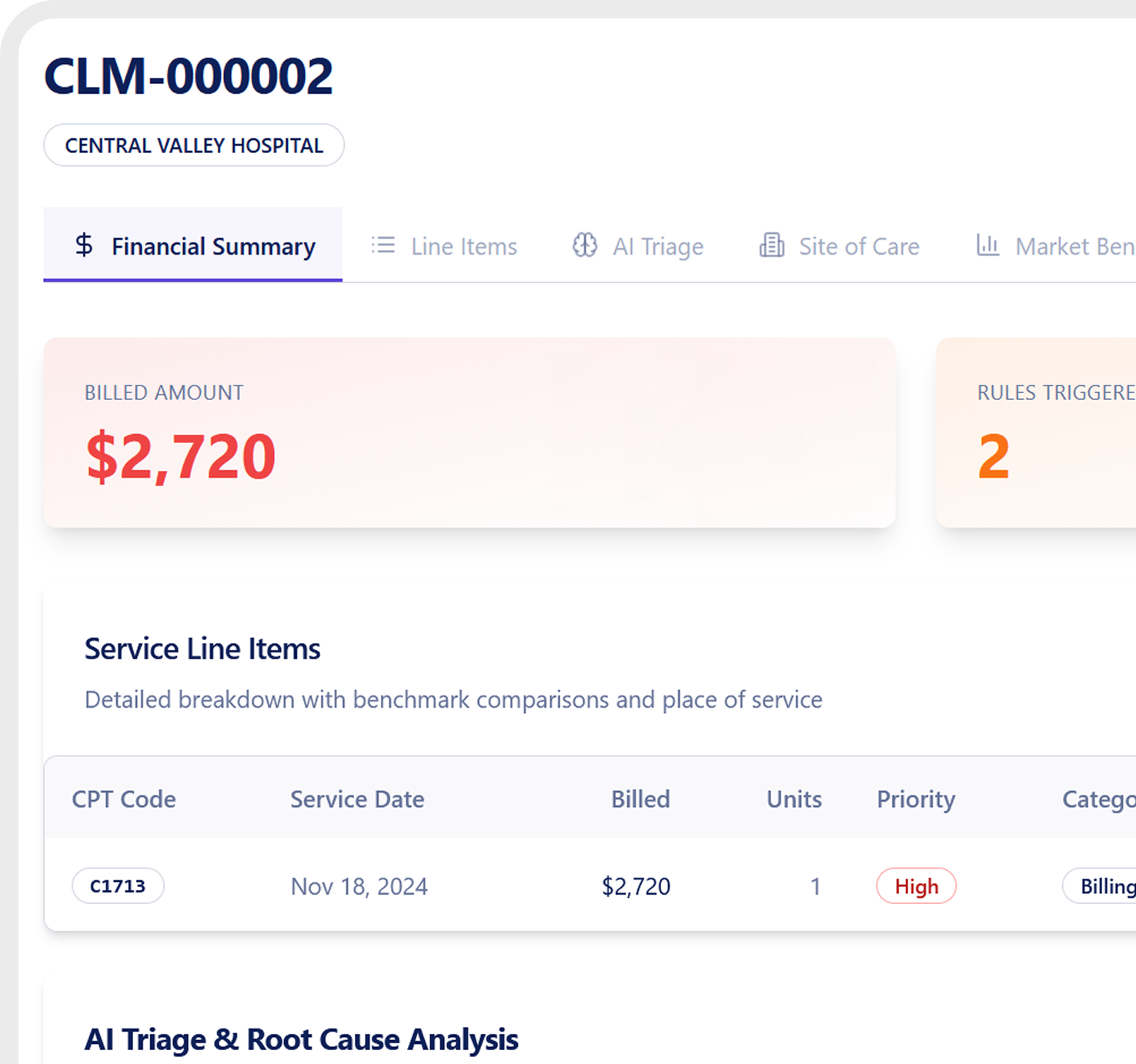
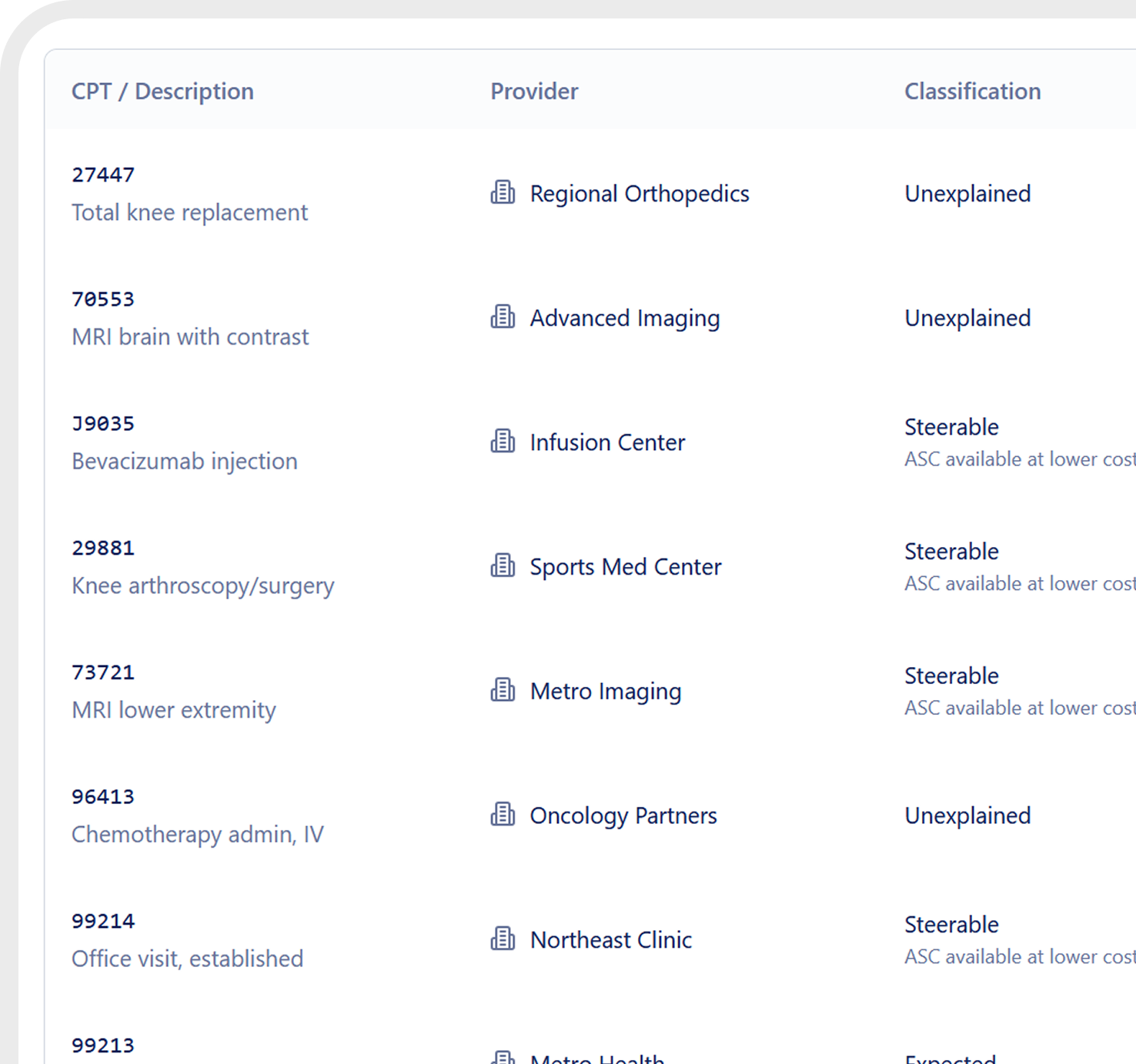
Reviews claims for pricing issues, unbundling, upcoding, and duplicate charges.
Price Transparency
Compares billed amounts against payer and hospital price data.
Focused Intervention
Only claims with real savings potential are routed for negotiation or action.
Real-Time Oversight
Employers and TPAs see claims in progress and savings impact in real time.
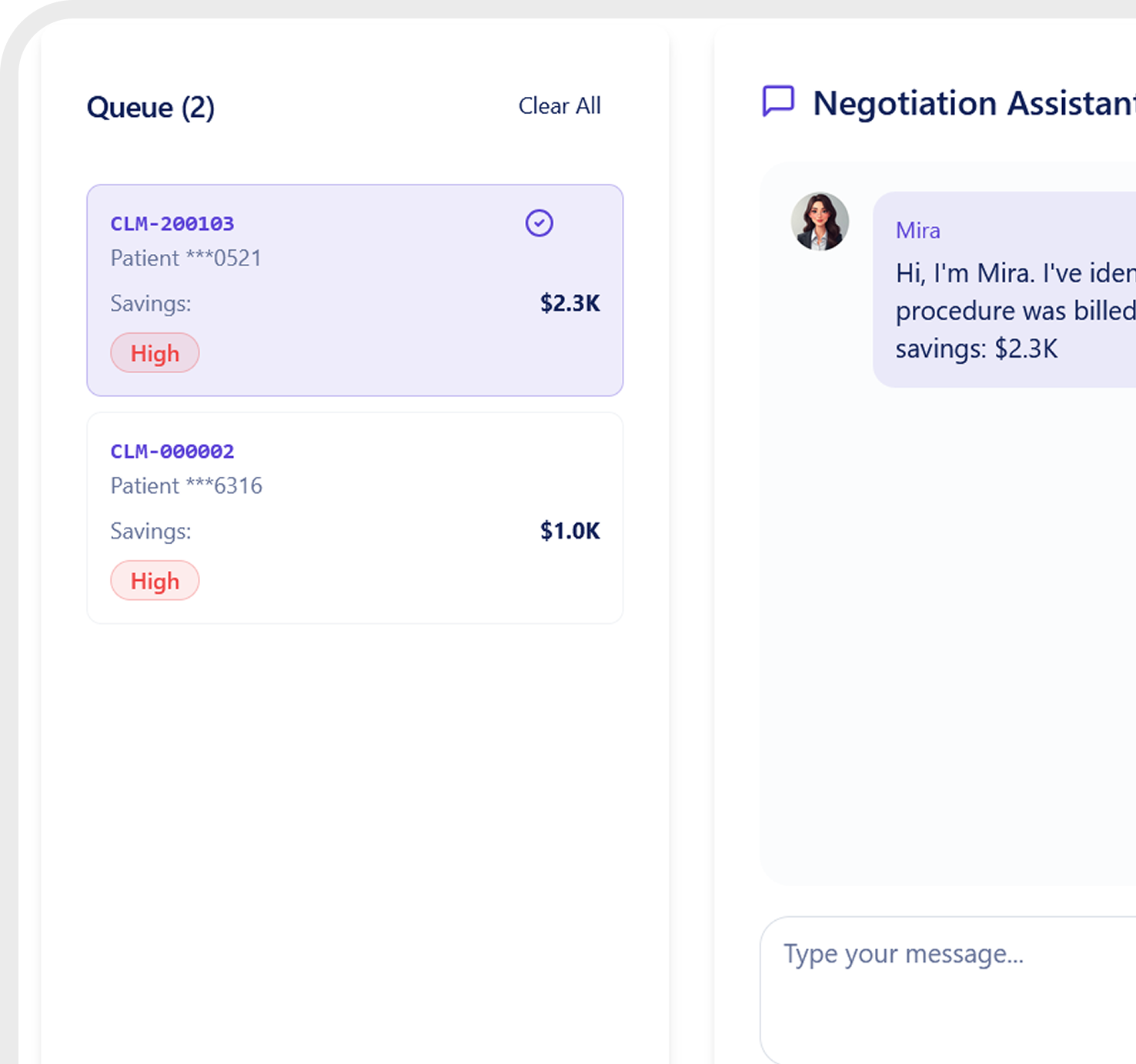
Claims Intelligence Powered by AI Agents
Every claim triaged, negotiated, and overseen before payment.
.png)
Mira
Reviews every claim and flags pricing, coding, and billing risks.
.png)
Nina
Prepares evidence to support claim correction and negotiation.

Theo
Provides real-time visibility, documented decisions, and savings impact.
Give TPAs and Employers Real Control Over Claims
Operational Oversight
See claims as they move through the system, not weeks later.
Cost Exposure Clarity
Understand where spend is accumulating and where intervention matters most.
Actionable Prioritization
Focus teams on high-impact claims instead of manual sampling.
Fiduciary-Grade Decisions
Support claims decisions with defensible data and documented rationale.
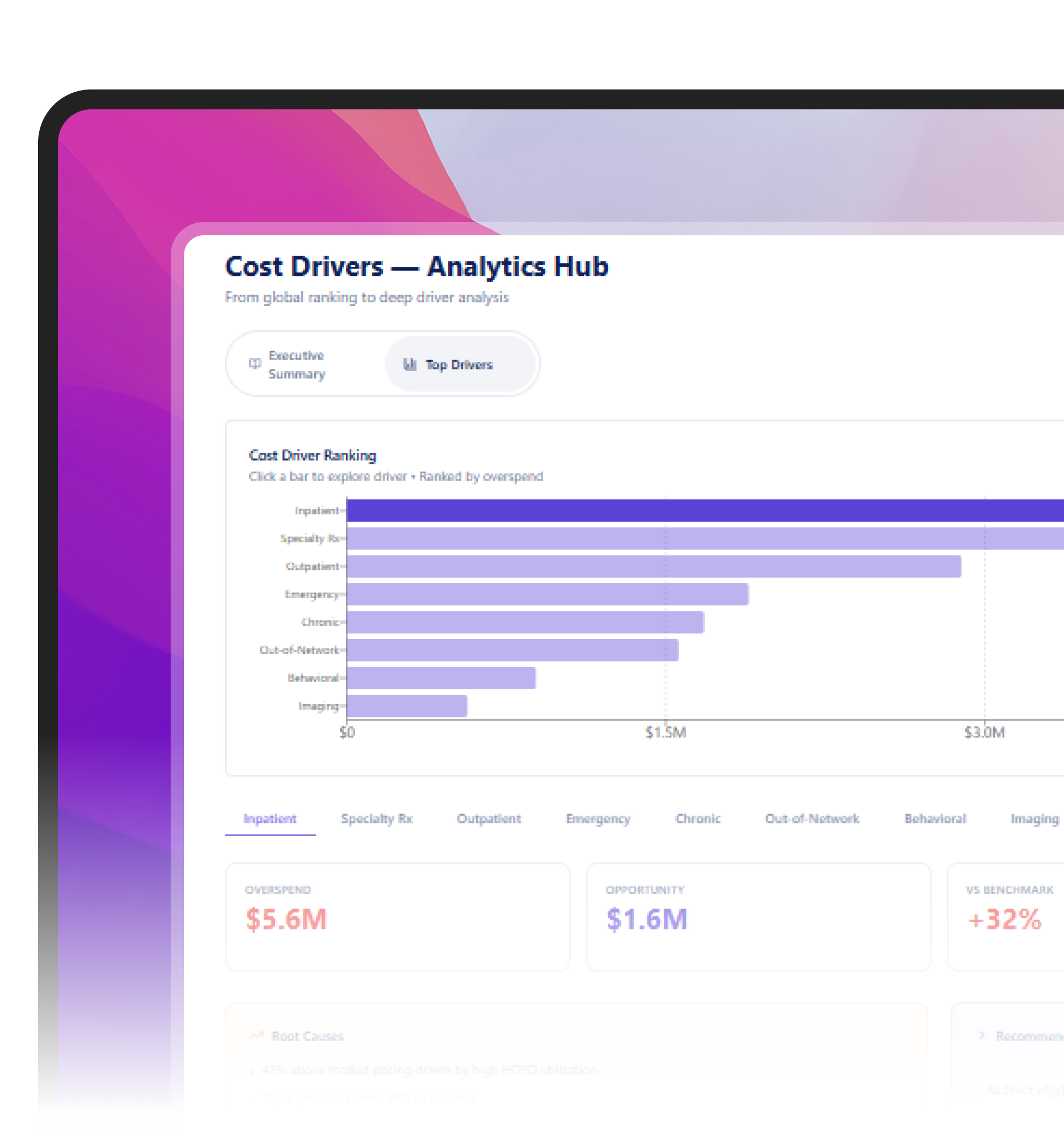
Claims Savings You Can Prove
Reduce up to
10%
of total medical claims spend through pre-pay triage and intervention
Triage
100%
of claims without adding analyst headcount
Save
>600K
in avoidable spend per 1,000 member lives annually
What Sets BenOsphere Apart
Capability
Real-time claim triage
AI + human intervention
Uses price transparency data
TPA-native workflowTPA-native workflow
Integrated with Slack and MS Teams
Complete stack
Simple pricing
Fast deployment (<2 weeks)
BenOsphere
Zelis
ELAP
Springbuk
Built on National Price Transparency Data
Uses payer and hospital pricing to validate claims in real time.





















































Your Questions, Answered
Still have some questions? Don’t worry. Take a look at our FAQ below.